Hospitals exist to heal people, but modern healthcare is also beginning to look beyond the walls of the operating room. Over the past few years, doctors and administrators have realized that patient care and environmental responsibility are connected. A major trigger for that realization has been the desflurane climate impact.

What used to be a routine anesthetic choice is now a topic discussed in medical conferences, hospital board meetings, and even public policy discussions. The desflurane climate impact has forced healthcare professionals to ask a difficult question: can medicine protect patients today without harming the planet tomorrow? Most patients never think about anesthesia beyond whether they’ll wake up comfortably after surgery. Yet what happens after the procedure ends matters too. The gases used during surgery don’t simply disappear they exit the hospital through ventilation systems and enter the atmosphere. When hospitals finally measured their carbon footprint, they discovered that operating rooms were responsible for a surprisingly large portion of emissions. That finding didn’t just surprise sustainability experts; it caught many anesthesiologists off guard as well. What followed has become one of the fastest practice changes in modern medicine.
The desflurane climate impact refers to the environmental consequences of releasing this commonly used anesthetic gas into the air. Desflurane became popular because it worked quickly and allowed patients to wake up faster after procedures. For decades, that efficiency made it a favorite choice in busy surgical centers. However, research later showed that its global warming potential is thousands of times higher than carbon dioxide over long periods. Hospitals now see reducing its use as one of the simplest ways to cut emissions while keeping surgeries safe and effective. Instead of abandoning anesthesia gases entirely, doctors are adopting safer alternatives and adjusting techniques, so less gas escapes into the atmosphere.
Table of Contents
Common Anesthesia Gas Linked to Climate Impact
| Key Aspect | Information |
|---|---|
| Anesthetic Gas | Desflurane |
| Medical Use | General anesthesia during surgery |
| Environmental Concern | Very high greenhouse warming potential |
| Relative Impact | More than 2,000× stronger than CO₂ |
| Atmospheric Duration | Persists in atmosphere for years |
| Main Alternatives | Sevoflurane, isoflurane, intravenous anesthesia |
| Hospital Response | Restrictions, education, and phase-outs |
| Patient Safety | No meaningful change in outcomes |
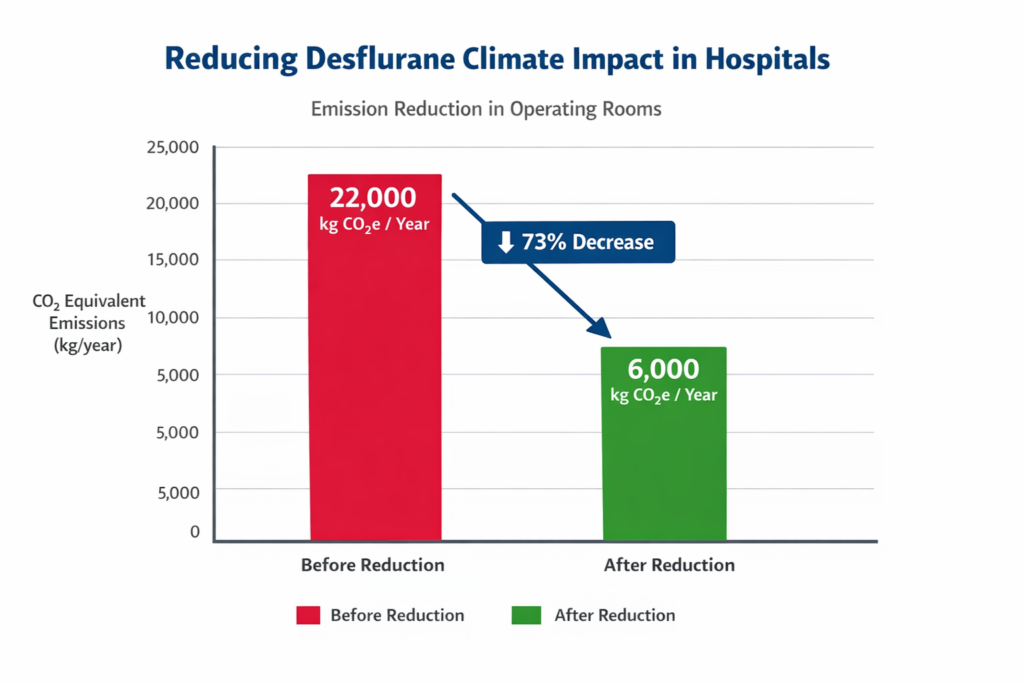
| Emission Reduction | Up to 80% reduction reported |
Medicine constantly evolves. New discoveries often change how doctors diagnose disease or perform surgery. Occasionally, they also change how healthcare interacts with the world outside the hospital. The growing awareness of the desflurane climate impact shows that even routine clinical decisions carry broader consequences. By choosing lower-impact anesthesia methods, hospitals protect both patient health and environmental health. This shift does not rely on futuristic technology or complicated systems. It comes from knowledge, responsibility, and professional judgment. Doctors still focus on safe surgery and smooth recovery, but now they also consider long-term public health. In many ways, the operating room has become a symbol of modern medicine’s future: healing individuals today while safeguarding the conditions that allow communities to stay healthy tomorrow.
Why This Common Anesthesia Gas Matters
- At first glance, the amount of gas used in a single surgery seems tiny. But scale changes everything. Large hospitals perform dozens of operations every day. Multiply that by thousands of hospitals across the world, and suddenly a small emission becomes a major environmental contributor.
- The desflurane climate impact is significant because the gas stays intact in the atmosphere. Unlike carbon dioxide, it is not easily absorbed by natural processes. Even a few hours of surgical use can equal the emissions of driving a petrol car for hundreds of kilometers. Once anesthesiologists understood this comparison, the issue became easier to grasp.
- Healthcare professionals are not environmental scientists, but they do understand responsibility. When they realized that a simple choice of anesthetic could dramatically affect emissions, many began voluntarily switching to other options.
Hospitals Change Course
- The transition did not happen overnight. Hospitals first needed reliable evidence showing that changing anesthesia practices would not harm patients. Clinical studies and real-world experience provided reassurance. Recovery times stayed the same. Complication rates did not increase. Patient satisfaction remained high.
- Once confidence grew, hospitals introduced new policies. Some facilities now require justification before desflurane can be used. Others removed it from operating rooms entirely. Education sessions became common, explaining how the desflurane climate impact compares to alternative drugs.
- Interestingly, the push often came from doctors themselves. Many anesthesiologists, after learning the environmental data, chose to modify their habits without being forced. The culture shift spread quickly because it aligned with the medical profession’s core values—do no harm.
Available Alternatives of Common Anesthesia Gas
Doctors still have several reliable anesthesia methods.
- Sevoflurane has become the primary replacement. It works similarly but produces far fewer emissions. Patients wake comfortably, and medical staff are familiar with its use.
- Isoflurane, an older drug, is also used in certain procedures. Although not new, it has a much lower warming effect than desflurane.
- Another option is Total Intravenous Anesthesia (TIVA). Instead of inhaled gas, anesthetics are delivered through IV medications. Because nothing is released into the air, the desflurane climate impact can be avoided entirely when this method is suitable.
- These alternatives demonstrate that environmental improvement does not require compromising medical care.
Patient Safety Comes First
- Whenever medical practice changes, safety is the main concern. Anesthesia affects breathing, heart rate, and consciousness. Doctors would never accept an environmental solution that risks a patient’s life.
- Fortunately, evidence shows that alternatives are just as safe. Surgeons report no difference in operation quality. Recovery rooms function normally. Patients typically have no idea which anesthetic was used.
- Desflurane still remains available for special situations where it offers a clinical advantage. The goal is thoughtful use, not total elimination. This balanced approach allows hospitals to address the desflurane climate impact while preserving medical flexibility.
Financial and Practical Challenges
- Changing practice always requires adjustment. Hospitals had to update training programs and revise surgical protocols. Some facilities also purchased equipment to support intravenous anesthesia methods.
- However, the financial results were unexpected. Desflurane is expensive, and reducing its use lowered supply costs. Ventilation systems also required less energy to remove excess gas from operating rooms. Over time, many hospitals saved money.
- This created a rare situation: environmental responsibility aligned with financial efficiency. Administrators who initially worried about costs became supporters once savings became clear.
Environmental Benefits
- Healthcare systems contribute a measurable portion of national greenhouse gas emissions worldwide. Within hospitals, operating rooms stand out because of anesthetic gases.
- After limiting the desflurane climate impact, some medical centers reported emission reductions equivalent to removing hundreds of cars from the road each year. That level of improvement from a single change attracted attention from policymakers and sustainability experts.
- Importantly, the solution did not require major construction or advanced technology. It relied on awareness and clinical decision-making. That makes it one of the most practical environmental actions available to healthcare facilities today.
A Broader Shift In Medicine
The discussion surrounding anesthesia reflects a larger change in healthcare thinking. Climate change affects respiratory illness, heat-related disease, and public health overall. Doctors increasingly see environmental protection as part of preventive care. Medical schools now include sustainability in training. Young physicians learn to consider environmental consequences alongside safety and effectiveness. The desflurane climate impact often serves as a real-world example of how small choices can create global effects. Hospitals are also reviewing waste disposal, single-use plastics, and energy consumption. The operating room has become a starting point for broader environmental reforms within healthcare systems.
FAQs on Common Anesthesia Gas Linked to Climate Impact
1. Why Are Hospitals Reducing Desflurane Use?
Hospitals are limiting it because the desflurane climate impact is extremely high. The gas traps heat in the atmosphere much more effectively than carbon dioxide, making it a significant contributor to emissions.
2. Is Surgery Still Safe Without It?
Yes. Alternatives such as sevoflurane and intravenous anesthesia provide the same level of safety and effectiveness for most procedures.
3. Will Patients Feel Any Difference?
No noticeable difference for most people. Recovery time, comfort, and surgical outcomes remain essentially unchanged.
4. Is Desflurane Completely Banned?
No. Some hospitals still keep it for specific medical cases where doctors believe it offers a clinical benefit.
















